Bundled payment episodes for major joint replacement (MJR) have been among the most successful "experiments" into the BPCI and CJR programs. Most BPCI participants in MJR episodes have been effective in reducing post-acute institutional utilization, and have achieved significant cost savings in these episodes. Among our clients participating in the CJR program, about 35% achieved savings that exceeded the stop gain limits; another 25% achieved savings that did not exceed the stop gain limits, and only 25% had losses. The trend factor used to adjust based BCI target prices has decreased more than 10% for DRG 470, indicating that national cost trends in this clinical area are significantly negative. While success in other clinical areas has varied, MJR episodes show almost universal success.
Outpatient TKA Surgery
But the potential for success in these episodes was significantly upended when CMS recently announced the removal of total knee arthroscopy (TKA) from the Medicare inpatient-only procedures list. This allows these procedures to be performed on outpatient basis, but also creates the presumption that they must be performed on an outpatient basis unless compelling contrary clinical evidence can be documented. The effect of this change is that a large number of relatively uncomplicated TKA cases will exit the CJR and BPCI Advanced programs because those programs do not include episodes initiated by TKA surgery when performed in an outpatient setting. The effect of removal of these lower-cost cases from these programs will be to increase the cost of the remaining episodes, which will then be compared to the existing targets. Unfortunately, these targets were derived from a population that included all TKA cases including those that would have been performed on an outpatient basis, so the target population no longer matches the performance period population. This results in targets that are much lower than they would have been had the targets been computed from a similar population, which therefore will create significant financial losses for hospitals who perform a significant percentage of these procedures on outpatient basis.
Effect on Episode Cost
To attempt to quantify this change in episode cost, Singletrack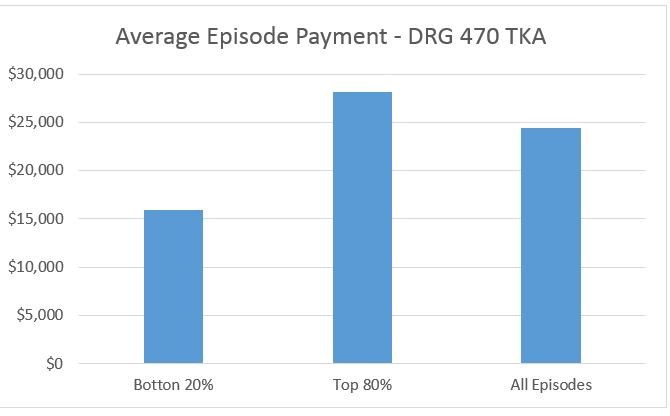 Analytics analyzed the effect on episode cost of removing the lowest cost 20% of episodes from a large population of CJR episodes in DRG 470, simulating the effect of moving 20% of these cases to an outpatient setting. The results of this analysis indicate that the outpatient-eligible cases have an average episode cost of almost $10,000 below the average of all episodes, while the 80% of episodes that would remain in an inpatient setting have an average cost about $4000 above the average of all cases. Assuming the target was equal to the average cost of all episodes, moving the bottom 20% of episodes into an outpatient setting would create an average loss of approximately $4000 per episode on all remaining episodes. This is obviously not an acceptable result for hospitals participating in these episodes in CJR or BPCI Advanced.
Analytics analyzed the effect on episode cost of removing the lowest cost 20% of episodes from a large population of CJR episodes in DRG 470, simulating the effect of moving 20% of these cases to an outpatient setting. The results of this analysis indicate that the outpatient-eligible cases have an average episode cost of almost $10,000 below the average of all episodes, while the 80% of episodes that would remain in an inpatient setting have an average cost about $4000 above the average of all cases. Assuming the target was equal to the average cost of all episodes, moving the bottom 20% of episodes into an outpatient setting would create an average loss of approximately $4000 per episode on all remaining episodes. This is obviously not an acceptable result for hospitals participating in these episodes in CJR or BPCI Advanced.
Can Targets be Adjusted?
A potential solution to this issue might be to attempt to adjust the targets to compensate for the loss of cases performed in an outpatient setting; however that adjustment would need to be established individually for each participant based on the percentage of that participant’s cases that are performed as outpatient. This is because the variation in outpatient surgery across hospitals is highly variable, and depends on patient mix, surgeon preference, facility availability, and other factors that cannot be determined from historical data. Therefore, the ability to CMS to make this adjustment, and the accuracy of the adjustment if CMS chose to do so, would be highly questionable.
No Gainsharing Waivers
The migration of TKA cases out of the BPCI and CJR programs would have other negative effects because those cases would no longer be eligible for the waivers that are part of those programs. In particular, gainsharing payments to physicians would no longer be allowable for TKAs performed in an outpatient setting, which would create a strong financial disincentive for orthopedists to perform any such surgeries on outpatient basis. Other waivers, such as the three-day SNF waiver and the ability to provide incidental benefits to beneficiaries will also be unavailable. Data on post-acute services, which is provided to BPCI and CJR participants, would not be provided for outpatient TKA cases, and the volume of the remaining inpatient cases would diminish, decreasing the statistical and financial stability of those episodes in those programs.
Expectations for BPCI Advanced
Because of these issues, we had hoped that CMS would include TKA episodes among those BPCI Advanced episodes that may be initiated by an outpatient surgery. Unfortunately, this is not the case. We realize that historical data for these cases is not yet available, but perhaps some surrogate could be developed that allow them to be included until sufficient volume of outpatient TKA cases can be accumulated to provide the basis for target computation. This would assure BPCI Advanced participants that they would not be disadvantaged by the expected migration of these cases to an outpatient setting.
Effect on Program Participation
But apparently none of this is occurring in either the CJR or BPCI Advanced programs. CMS’s only comment on this issue is that they are considering potential options. Meanwhile, participants in voluntary MSAs in the CJR program, even those with strong financial results, are electing to exit that program because of the uncertainty over this issue. And while most participants in MJR episodes in BPCI and CJR have achieved financial success, the level of uncertainty over this issue causes us to recommend that no episode initiator should participate in the Major Joint Replacement of Lower Extremity episode in the BPCI Advanced program. While the clinical structure of these episodes make them a prime candidate for care redesign, the uncertainty around the establishment of target prices creates too much risk.
